Ministry: We’ve paid Sh8.4b NHIF debts

More than 8,000 health providers contracted under the defunct National Health Insurance Fund (NHIF) have received an estimated Sh8.4 billion between October 1, 2024 to date when the Social Health Authority (SHA) took over.
This emerged yesterday as the government formally kicked off the verification process of the Sh33 billion debts incurred between 2021 to September 30, 2024. During this period NHIF had contracted and enrolled 8,886 healthcare providers (HCPs).
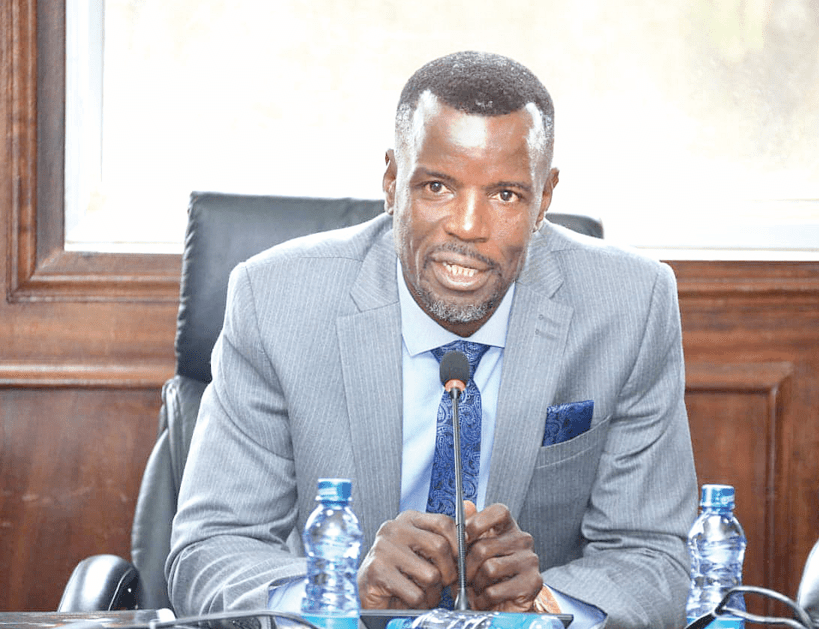
The revelations were made by outgoing Medical Services PS Harry Kimtai at Afya House, where he moderated a session which saw Health Cabinet Secretary Aden Duale inaugurate a 13-member NHIF Pending Medical Claims Verification Committee.
Chaired by James Masiro Ojee and deputised by Dr Anne Wamae, the Committee is mandated to scrutinise and analyse the existing NHIF pending medical claims that have accumulated between July 1, 2022 and September 30, 2024.
Given strictly three (3) months to complete the task, the committee will also be required to recommend to the Ministry on the mode of settlement.
“The government started paying health providers in October, with Sh8.4 billion already released,” he said.
The PS who was moved to the Mining docket in the recent Cabinet shake-up is currently acting on behalf Dr Ouma Oluga pending his vetting by the National Assembly.
Kimtai said to complete the payments as claimed by the health providers, there was need for verification.
Pending bills
Those facilities, according to the PS, are supposed to be paid and the process is on. He said about 91 per cent of the facilities share around Sh5 billion of the entire pending bills.
“Now the Sh10 million and above each are the ones that are subject to verification which then will clear the air in terms of whether these were fraudulent claims or genuine,” he said.
Established through Gazette Notice No. 4069 of March 28, the committee is also mandated to establish a clearly defined criteria for detailed examination and analysis of such pending medical claims with a view to determine the genuineness of each.
It will also be required to make recommendations to the Ministry on the necessary actions to be taken for satisfactory disposal or settlement of the identified pending medical claims.
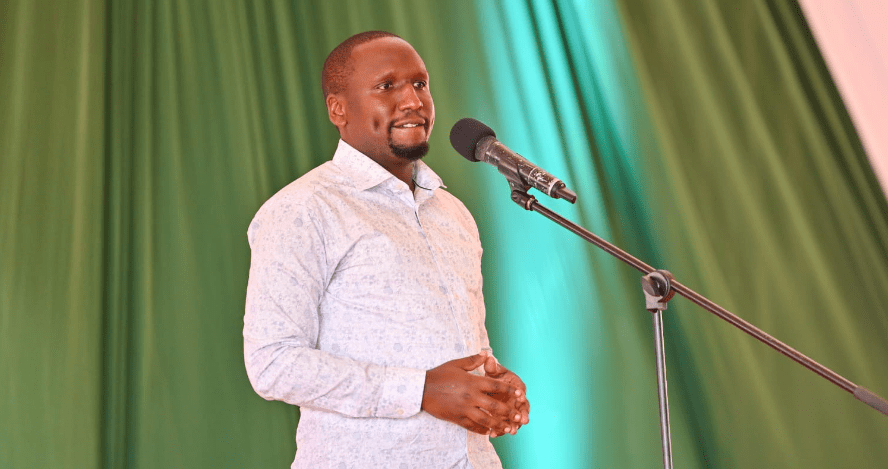
While expressing confidence in the newly inaugurated team because of its diversity in membership, Duale challenged the Committee to carry out a thorough and objective review of all outstanding claims and recommend payment only to the genuine ones.
He emphasized that although the Government is aware of the financial challenges facing some healthcare providers, transparency, accountability, and value for money must remain central to the verification process.
“This Committee is a critical step towards restoring public trust in the health financing system. We must ensure that every shilling spent delivers real health outcomes, in line with the Government’s commitment to Universal Health Coverage under the Bottom-Up Economic Transformation Agenda (BETA),” the CS stated.
The committee is also expected to identify any cases where there may have been corrupt, fraudulent and fake medical claims and make appropriate recommendations to the relevant government agencies.
Payment plan
Duale tasked the Committee to make recommendations to the MoH on the necessary actions to be taken for satisfactory disposal or settlement of the identified pending medical claims, and also propose reforms or measures that will ensure, or prevent the recurrence of unverified or accumulated claims in the future.
“The President, directed the government to pay all hospitals with total claims of Sh10 million and below in full, representing 91 percent of all facilities that were contracted by NHIF,” the CS announced, pointing out that the remaining nine per cent of the hospitals with total claims of above Sh10 million, will be subjected to a verification exercise to be completed within 90 days after which a payment plan will be agreed upon.