Expert calls for tracing of genes to fight cancer
A Kenyan doctor says there is need to start tracing genes of Kenyans if the country is to win the war against cancer.
Speaking to People Daily, Dr Njoki Maina says in understanding “our unique DNA (deoxyribonucleic acid) as Kenyans” we can start treating various cancers using targeted medication, from an informed point of view.
Njoki, who is a senior lecturer at the University of Nairobi and working closely with various PhD students on research projects, some focusing on solving the cancer outbreak puzzle, says it is important for researchers to focus on mapping of the genes to offer firm evidence that a disease transmitted from parent to child is linked to one or more genes.
She says this would provide clues about which chromosome contains the gene and precisely where the gene lies on that chromosome.
“We must go back to the genome and work backwards to eliminate this scourge,” she says, adding that Uganda is already working on such a project.
Cancer is a genetic disease caused by changes in DNA that control the way cells function, especially how they grow and divide.
It is the third leading killer disease in Kenya claiming 32,987 lives annually according to the 2018 Global cancer Observatory (Globocan) report.
A genome is an organism’s complete set of DNA, including all of its genes whereby each genome contains all information needed to build and maintain the organism.
Experts say they can be inherited, but most arise randomly during a person’s lifetime, either as a result of errors that occur as cells divide or from exposure to DNA-damaging carcinogens. Every cancer has a unique combination of genetic changes and tumour DNA sequencing—sometimes called genetic profiling or genetic testing—is a test to identify the unique DNA changes.
Dr Maina says cancer genome sequencing can be used to provide clinically relevant information in patients with rare or novel tumour types.
While translating sequence information into a clinical treatment plan is highly complicated, it requires experts from different fields, and is not guaranteed to lead to an effective treatment plan.
“We must get the African genome sequenced, compare it with the Caucasians and then look for any outliers,” she says.
Our genome as Africans she notes is not unique per se’ but due to environmental, geographical, nutritional and climatic differences with Westerners, there is a high chance of genomic differences, which could go on to explain Ca therapy response, considering the drugs were tested on Caucasians. It would be great to enjoin our samples in such trial studies.
Skewed decisions
Also if the cancer is genetic, genetic screening can pick on the changes which predispose to a specific cancer. Intervention would save the person for example, Angelina Jolie had a mastectomy and removal of ovaries to avoid Breast/Ovarian cancer, a familial cancer.
This was after mutations in the responsible tumour suppressor genes were discovered. So even in familial cancer, the disease can be arrested or early intervention applied.
She observes that Africans have a unique genome which predisposes them to HIV/Aids as an example that informs the need to map genomes for Africans. Unfortunately, priorities in planning and skewed decisions avail very little resources to tackle the disease.
For example, it is not until three years ago when the National Cancer Institute (NCI) was constituted. However, since its formation, the institute is yet to be allocated any staff.
In a report presented to the National Assembly Health committee, it emerged that NCI is not facilitated well to take up its role, and it is not even in charge of the Sh14 million given to it as a grant.
“The inaugural board was not in control of the allocated funds as they were channelled through a department within the ministry,” reads the July 25, report in part.
Many countries are working on early detection of the disease. There is hope that cancer can be managed. But Kenya must set aside more resources to help leverage research into decision-making on the scourge.
A recent research showed that blood test can detect whether a person has lung cancer or not before symptoms develop. The research on people who were at high risk of developing the disease indicated positive results in a random controlled trial in Scotland. The experts on early detection of lung cancer found out that people who took the test were more likely to be diagnosed with the illness four years or more before standard clinical diagnosis.
A new research presented at the World Conference on Lung Cancer in Barcelona, Spain also says a new immunotherapy cancer drug boosts survival rate five-fold, according to scientists from Yale.
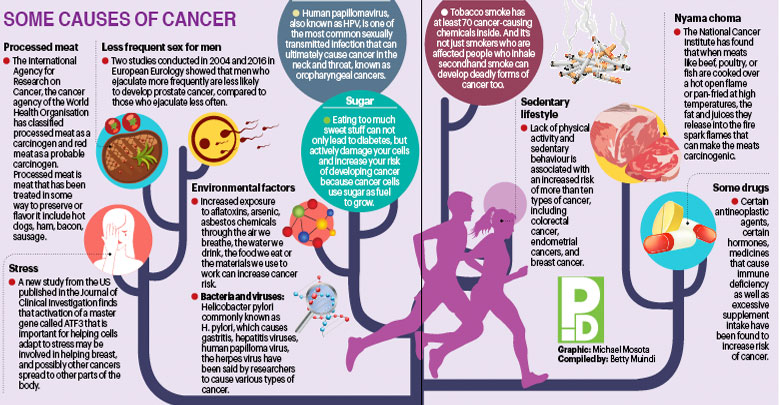
Environmental factors
Dr Maina points out two things; the disease can be caused by genetics and environment. This is informed by the food we eat and carcinogens in our environment,
We can not do a lot about genetics, especially if it’s inherited mutations—abnormal cell changes—for lack of a better word. But we can achieve a lot by taking care of our surrounding environment.
“Let’s not go down without a fight,” she says. The scourge has spread fear among Kenyans and upon diagnosis trauma can easily make them succumb within a short time.