State alters treatment for elderly patients with HIV
The government is changing the treatment model for ageing people living with HIV.
Consequently, it is beginning to be more concerned about this population as it could also be battling other chronic diseases that need immediate attention alongside HIV interventions.
At the heart of the proposed model, is a need for integrating HIV service delivery with other diseases.
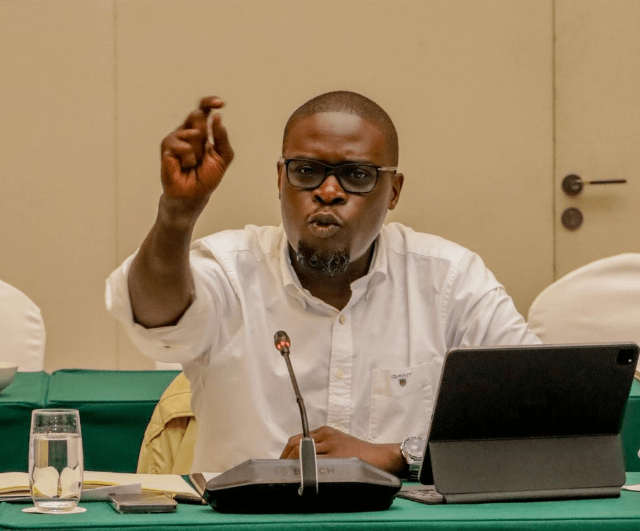
A stakeholders meeting hosted by the National AIDS and STI Control Program (NASCOP) in Mombasa heard that rather than focusing on the disease, the target will be more of the person.
According to health experts, a larger proportion of people living with HIV, and are advancing in age, are more likely to have co-morbidities, conditions that may come over and above HIV.
“For example, close to 40 per cent may have hypertension or hyperpressure, about nine per cent may have diabetes, but up to 60 per cent have what we call osteoporosis, this is when the density of the bone goes down so the bones are likely to break,” Dr Loyce Ombajo, an infectious disease expert with Kenyatta National Hospital said.
She noted that a large proportion of people living with HIV, have osteoporosis and also close to 40 per cent may have a decline in how the kidneys are working.
The experts are arguing that the HIV landscape has changed since it was declared a national disaster 20 years ago. What followed was the establishment of structures and approaches that were specific to the disease, and up to now, the government and partners feel that as a country, Kenya has reached a point of epidemic control and normalised.
However, according to Elgeyo Marakwet CEC Member in charge of Health and chairman of the Health CECs Caucus in the country Michael Kibiwott, since HIV is here to stay as a chronic disease, the government and partners, feels that it’s high time a change in the way things have been done in the past is needed.
Common goal
He said that a common goal of tackling these conditions is needed.
“In this conference we are exchanging ideas on how we can integrate HIV services to others, so that we can avoid duplication, but achieve synergy of doing things together,” he said, explaining that this needs to change urgently to manage what may likely cause death to human beings other than HIV.
For instance, the HIV programming that has happened before, where you will have Human Resource that’s specifically focused on treating HIV; digital services, for example, electronic records that were particularly on HIV, lab services that were specific to the disease, building infrastructures that were comprehensive care centres.
However, according to Kibiwott, this has changed now since there are HIV patients who are living longer, ageing and contracting other diseases such as diabetes, High Blood Pressure, various cancers and other NCDs that were not there.
“Therefore, there is a need to approach the next strategy holistically by delivering services that don’t tackle only HIV but affiliated conditions,” he stated.
Prof Sylvester Kimaiyo, a lecturer at Moi University and Moi Teaching and Referral Hospital in a programme called AMPATH- Academic Model of Providing Access to Health, the main government partner in the new strategy, says integrating HIV Services is cost-effective and will address other conditions.
“There are four main NCD co-morbidities related to HIV: cardiovascular disease (CVD), depression, diabetes and cancer. Integrating NCDs in the HIV response not only provides better health outcomes for a person living with HIV and NCDs but it is also cost-effective,” he said while responding to questions from journalists at the HIV Service Delivery Integration Summit in Mombasa hosted by the NASCOP.
He called on the Ministry of Health and NASCOP to redesign HIV delivery services to respond to the multiple needs that a person living with HIV - alongside other comorbidities that come with old age - requires navigating the conditions beyond the disease services.
Nascop Chief Executive Officer, Dr Rose Wafula said that in the context of the current epidemic response, there are about 1.3 million Kenyans who are accessing care in the health facilities, majority of whom, who access services at the primary healthcare, over 90 per cent from Level two to four. This population also, she said, over 65 per cent are aged above 35 years.
“This combination therefore tells you that beyond HIV, they have other health needs.
High risk
“So the service delivery integration is really a focus on the person rather than just a person at high risk,” she said, noting that along with integrating the HIV Service Delivery, the Ministry is also aiming to eliminate the stand-alone facilities because of the stigma and labelling associated with them.
Currently, in terms of location, Dr Wafula said establishing stand-alone facilities that are labelled HIV clients will not be there in the future as they aid stigmatisation.
“In future, these stand-alone facilities will not be there, because of the stigmatisation and discrimination that comes with it.
“We will have facilities where integrated services will be offered, without necessarily labelling. So we look to a future where there will be less stigmatisation and labelling,” she said.
In terms of HIV treatment, Dr Wafula noted that the country has a very good program, with set guidelines on how to manage HIV.
Most of the treatment of HIV comes as a single chapter for most patients and this single chapter is a combination of three different medicines.