NHIF on the spot over irregular claim payments
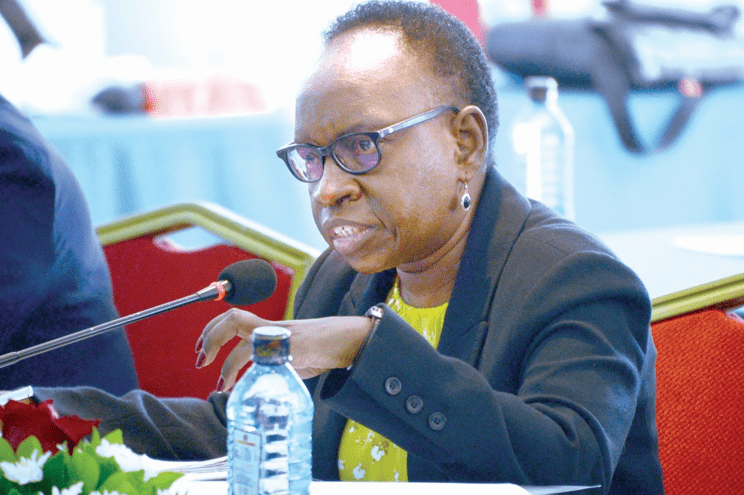
Auditor General Nancy Gathungu has unearthed massive irregularities in how the National Health Insurance Scheme (NHIF) paid out claims to beneficiaries amounting to billions of shillings.
In her latest report for the year ending June 2023, Gathungu revealed that hospitals billed more than the claims made by patients besides health providers irregularly making claims from the fund.
The audit also established that there were duplicate claims of various health schemes while surgical expenditure was done before peer review was done by doctors. It also established that there are duplicate payments for Ceasarean sections and normal deliveries.
Reads the report: “In my opinion, because of the significance of the matters discussed in the Basis for Adverse Opinion section of my report, the financial statements do not present fairly, the
financial position of the National Health Insurance Fund as at 30 June 2023 and of its financial performance and its cash flows for the year then ended.”
In the report, Gathungu raised concerns that there was unexplained overpayment on National Health Scheme Expenses amounting to Sh462.2 million.
Various schemes
The overpayment was made in respect to various procedures done including major surgery which was over paid by a whooping Sh285.8 million, Minor Surgery Sh29.4 million CT-scan Sh94.8 million, Basic Chemotherapy Sh25.6 million.
Others are normal delivery Sh1.3 million, c-section Sh1.3 million, rehabilitations 3.3 million, specialised surgery Sh3.6 million, MRI Sh16.1 million and complex chemotherapy Sh768,000.
Reads the report: “The statement of profit or loss and other comprehensive income reflects National Health Scheme expenses balance of Kshs. 34,362,413,090. However, the amount includes payments of Kshs. 963,737,709 while their specified limit was Kshs. 501,561,060 resulting in unexplained overpayments of Kshs. 462,176,649.”
It adds: “In the circumstances, the accuracy and completeness of the National Health Scheme expenses of Kshs. 963,737,709 could not be confirmed.”
On various schemes contracted by the fund, the report raises concerns that the hospitals billed Sh447.1 million against claims paid amounting to Sh814.9 million resulting to unexplained variance of Sh367.8 million.
The report notes that although the management attributed the variance to typing errors made by hospital clerks while inputting bill amounts in the E-claim system, there was no evidence of reconciling the billed amount to claims paid or requests for refunds for overpayments.
Among the schemes that were overpaid include the National Police Service/Kenya Police Service scheme which was overpaid by Sh16.2 million, National Health Scheme (NHS) Sh205.9 million, Universal health coverage (UHC) Sh47.6 Million, civil servant scheme Sh6.5million, Edu Afya scheme Sh24.1 million, Health Insurance Subsidy Program(OVC) Sh8.6 million, Health Insurance Subsidy Program (OPPSD) Sh3 million, county scheme Sh661,771, parastatal scheme 638,700 and Linda Mama Scheme Sh54.9 million.
Reads the report: “In the circumstances, the accuracy, completeness and regularity of the claims paid amount of Kshs. 814,893,467 could not be confirmed.”
The report also raises concerns that duplicate payments were made for ceasarean section and normal deliveries.
The report notes that in the case of Linda Mama programme, there exists an amount of Sh5.7 million paid to NHIF accredited hospitals whose analysis revealed 656 duplicates case code on caesarean section deliveries procedures carried out on the same patient.
Admission dates
An analysis of claims payment schedules revealed an amount of Sh247 million on duplicate payment of claims in respect to National Health Scheme at Sh221.4 million and Indigent’ Sponsorship (GOK) Program at Sh25.6 million.
Further, the report shows that there exists duplicate claims with same medical procedures, on the same admission dates but with different discharge dates in respect to 1,009 claims amounting to Sh9.96 million.
The report also shows that there exists another amount of Sh51.1 million for four schemes incurred on payment of 2,808 claims where the same patient was admitted in different hospitals at the same time.