How rare hereditary disease plagues my life
Harriet James @harriet86jim
Since she was five years old, Patricia Karani would have frequent allergic reactions, stomach upsets and swellings on her face, hands and limbs that the doctors failed to diagnose.
The swellings were not painful; the only time it hurt was when she handled something using her swollen hand.
“The swelling was so huge, they painfully pushed against my bones. It was an even progressive swelling, not lumps which became even more frequent in high school,” she narrates .
The frequent swellings forced her parents to transfer her to a school closer home despite the stellar performance that saw her enroll into a good boarding school.
In her later years, Patricia realised stress triggered the swellings. She would get swellings after two months, which would take five days to go down. Unfortunately, the medication she was given didn’t help.
“I was put on hydrocortisone (steroids that treats different skin conditions) and it was so expensive, my family had to give out the title deed as security for my treatment when I was admitted to hospital for a week.
I was put on constant antihistamines, which helped with the allergies, but there were swellings that did not respond to the same medication and doctors didn’t know the cause,” she recalls.
For the next 10 years of her life, Patricia was constantly on medication, but the swelling never stopped. She also experienced side effects, including hair growth, continuous mood swings and breaking of voice.
Deeper layers
The once high-energy person had to tone things down because strenuous work would cause swelling.
Consequently, she was forced to cancel events and dates, and her friends didn’t know what was wrong.
The condition also impacted on her job, as she could not keep asking for permission from work every time because of the swelling.
“After a long relaxing weekend, I would end up being sick on Monday and I had to keep on lying to my boss why I wouldn’t be able to go to work for five days.
As soon as I get better, I would overwork myself to finish my duties, which would result in stress that later on triggered the swellings,” she recalls.
In 2000, Patricia’s brothers, who also exhibited the same symptoms, travelled abroad in search of treatment.
Eight years later, Patricia finally discovered the cause of the swellings, marking a huge turning point to her life. She was suffering from hereditary angioedema (Hae).
Hae is the swelling of the deeper layers of the skin— a condition that results in recurrent attacks of severe painless swellings, which mostly affect legs, face, arms, intestinal tract and airway.
In cases where the intestinal tract is affected, there may be abdominal pain and vomiting.
Without preventive treatment, such swelling occur after days or weeks. Swelling of the airway might result in its obstruction.
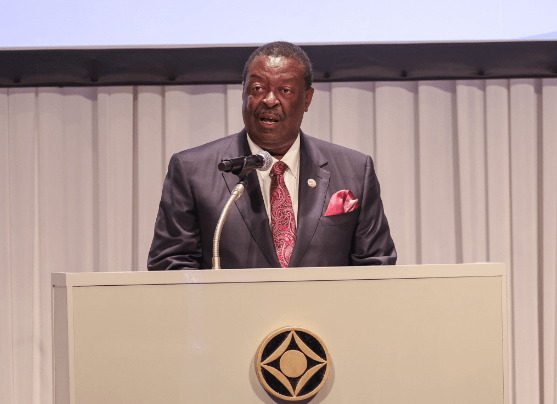
Dr Priya Bowry, an allergist, says swellings related to hereditary angioedema are different from swellings caused by allergy because of the mechanism through which the reaction occurs.
“In hereditary angioedema, the body produces bradykinin, a powerful chemical that causes swelling.
In allergic reactions, the body produces histamine, which causes itching, rushes, swellings, upper airway allergies, blocked nose and sneezing,” she notes.
Life threatening
In hereditary angioedema, when the body meets a trigger such as trauma, stress or infection, it sets off a reaction; however, there is no breaking mechanism to make it stop.
While swelling from allergies can last a shorter time, the ones from Hae can last for a few days without resolving. Some patients with the condition can get a flat non-itchy rash before the symptoms.
“In most instances, the body has a way of controlling reactions, but the lack of a special enzyme results in uncontrolled production of the chemical responsible for the swelling.
The swellings may affect the back of the throats and can result in death through asphyxiation (chocking of the air waves). Similarly patients get swellings in their stomachs and abdomen, making them suffer a lot as the reactions can last for many days and sometimes can be life threatening,” notes Dr Priya.
Currently, there are approximately 700 patients suffering from Hae in the country.
Patricia discovered the swellings run in the family and although her late father passed away from a different disease, he used to get the swellings.
Her late grandmother died from swelling in the voice box caused by Hae and her brothers too had the swellings, although they all experienced different triggers.
Diagnosing Patricia’s case was more complicated as she had an element of both allergy and Hae.
Despite having bouts of abdominal pain and life threatening laryngeal swellings in her early childhood, Patricia discovered, in her early 30s, intestinal swellings were the cause of severe abdominal pain.
No cure
“Swelling is the predominant symptom. Family history is also another way a person can know that they have the condition.
Finding the trigger is always a 50-50 chance. If we give antihistamine or steroids, these patients will not respond to them,” says Dr Priya.
There are three types of HAE, differentiated by levels and functionality of a protein called C1 inhibitor. In type one, there is low level of C1 inhibitor resulting in high production of bradykinin.
In the second type, the C1 inhibitor might be present, but it’s dysfunctional or not working properly.
The third type, which is the difficult one to diagnose, occurs when there is a mutation in one of the genes.
“The third type is more predominant in women in their late 30s and 40s, while type I and II tend to begin from childhood onwards,” Dr Priya says.
Hormonal stresses such as pregnancy, periods, menstruation or contraception can trigger the condition.
Because of its complexity, Dr Priya advises doctors to be careful and work it out systematically and give the correct diagnosis. The challenge with such conditions is the lack of correct treatment.
Though the condition has treatment and is manageable, it has no cure. Unfortunately, effective emergency medications are not readily available in the country and patients suffer adverse side effects from currently available medication.
“There are drugs available to control and prevent an acute reaction. In the first type of Hae, patients have to take treatment as prophylaxis to avert reaction or to be treated if you have an acute reaction.
There are a number of different prophylaxis and most of them are not available in the country at the moment.
The ones present, can be taken daily to prevent an attack,” says Dr Priya.
Lifestyle changes are also a major way to manage the condition. Dr Priya advises patients to find out what triggers the swellings and adjust their lives based on what affects them.
“One can use prophylactic treatment before visiting a dentist because the trauma caused by dental work can trigger severe swelling.
If you know that walking for many hours is going to cause swelling, then avoid it.
Sometimes, you can’t predict what’s going to happen, but just be mindful or aware of the condition and learn to manage your life around the trigger,” she says.
Dr Priya believes there needs to more awareness so that doctors can recognise the condition.
She also advises people who suspect to have the condition not to be shy to come forward for testing.
“More knowledge on the doctors on this condition will eliminate the many unnecessary tests and surgeries, which patients are subjected to before proper diagnosis,” she concludes.