Attention disorder opened my eyes to mental health
As one of the invisible disabilities, Attention Deficit Hyperactivity Disorder is not openly talked about, causing delayed diagnosis and treatment as Dannish Odongo and Sylvia Moraa found out
In retrospect, the signs were there all along. Dannish Odongo always struggled with insomnia as far back as he can remember.
He was incredibly fast in getting tasks done and grasping new information. He could feel emotions so deeply and had trouble concentrating, especially on things that did not interest him.
“While in school, I was restless and wondered why we had to have long lessons while we could learn within a shorter period.
It was the same case at work. I couldn’t understand why I had to work all day while work could get done within few hours,” he says. Ultimately, he knew he was different, but didn’t’ know how.
Yet it took 31 years before someone linked his symptoms to Attention Deficiency Hyperactivity Disorder (ADHD).
The diagnosis was made by a psychiatrist Odongo had begun seeing in December 2018 in the aftermath of a tough season in his life.
He had just come out of a three-year relationship that had left him emotionally drained, was dealing with trauma of covering the 2017 general elections as a reporter in a local media house and had resigned from his job as a reporter in March 2018 and joined another organisation in a demanding position.
For months after the break-up, he experienced persistent fatigue, insomnia and had nightmares.
Then one day in December 2018, he walked into a clinic in Upper Hill hoping to get medication to help him manage the insomnia. But tests revealed the problem was deeper than he had thought.
Along with the shocking ADHD diagnosis, Dr Frank Njenga, a psychiatrist, also said that Odongo had depression and Post-traumatic Stress Disorder.
“The doctor simply looked at me and said, let me show you a place you can go and rest,” says Odongo.
So, he went home, packed his bags and checked into Bustani Mental Health Hospital in Lavington where he stayed for six days undergoing therapy.
Leaving the health facility after treatment, it’s as if a switch had been flicked. “For the first time in my life, my mind felt quiet and peaceful. A lot about the person I was, made a lot of sense,” he says.
Though it took so many years, Odongo considers the ADHD diagnosis a blessing in disguise.
It’s because of that diagnosis that he took time to heal from various traumas he had accumulated over the years.
The diagnosis also changed his perspectives about mental health issues. In the one week he was in therapy, Odongo took time to extensively research about mental health conditions.
The ADHD diagnosis and the realisation of the co-morbid conditions (condition that occurs with another at the same time) including depression opened his eyes to skewed cultural views of mental health.
Having a mental health condition in the African society for instance earns the patients the tag of being ‘mad’.
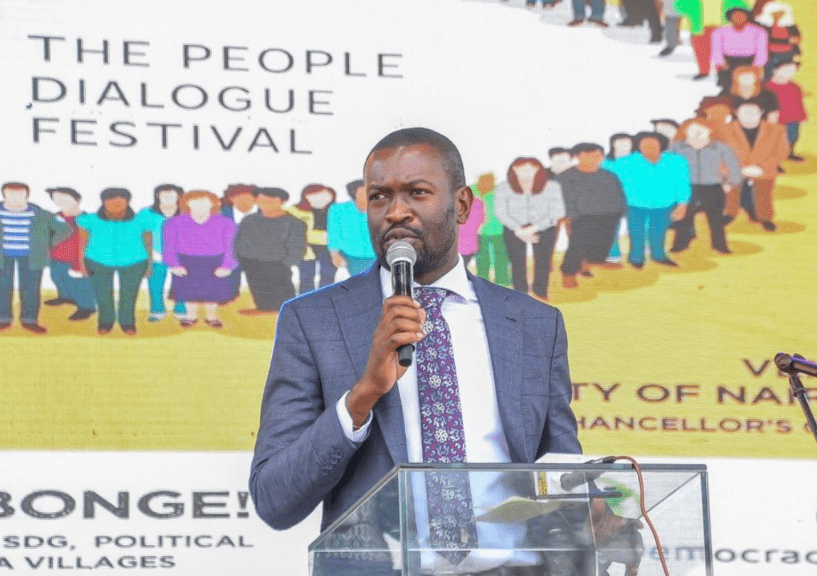
These gaps in knowledge are what motivated Odongo to immerse himself in creating awareness and changing perceptions as a mental health advocate.
For Sylvia Moraa’s eight-year-old third-born son, Bradley, the ADHD diagnosis came comparatively earlier. He was diagnosed when he was one.
Moraa did not suspect anything was the problem when he delayed to crawl, walk and with his speech. She had noticed all these delays, but thought that he was mimicking his older brother.
“My second-born son, Andrew, who is autistic, had similar delays and so I comforted myself that Bradley was just trying to be like his brother,” she says.
Perhaps Bradley’s diagnosis could have been delayed were it not for the doctor’s insistence, upon carrying out assessments for Andrew, on testing him as well.
The early diagnosis helped Moraa initiate him into treatment and have improved health outcomes.
“He is now undergoing therapy and there has been significant improvement,” says Moraa.
Dr Alliya Mohamed, a paediatrician says ADHD is a neurodevelopmental disorder that can either manifest symptoms in childhood or can be detected later in life.
Research has found the condition, characterised with impulsiveness, inattentiveness and hyperactivity, to be more common among boys than girls.
According to the Royal College of Psychiatrists as many people get older the condition improves, and around one per cent of patients continue to have the condition with two to four per cent having partial symptoms.
ADHD symptoms are often confused with mood disorder, anxiety and other conditions with overlapping signs, hence may go undiagnosed for long periods of time.
Adults with ADHD are likely to have anxiety disorder, depression or other co-morbid conditions.
Dr Mohamed says proper management of the condition preferably using a multidisciplinary approach including parents, teachers, doctors and therapists, ADHD patients can have a better quality of life.
For both Odongo and Moraa, one of the biggest frustrations in dealing with the condition is the segmented approach accorded to such disorders.
“I now realise it is time we looked at these health conditions from an all-rounded perspective. It’s not just a health, but also largely a social issue.
High unemployment rates, poverty, toxic political environment are among the many possible mental health triggers in our population that need to be addressed,” says Odongo.
Moraa adds that the stigma from the community to patients with neurodevelopmental conditions and their caregivers may trigger mental health conditions.
“Navigating around this condition as a patient or a caregiver is not easy. It’s sometimes so frustrating because there are no well thought out support services for such conditions.
Some parents taking care of children with such a condition are pushed to the point of even committing suicide,” says Moraa.