Stop scapegoating care workers in Covid fight
Simon Johnson and Larissa Lucas
After a two-year pandemic, with the Omicron variant raging and uncertainty ahead, there is an understandable desire to blame someone for the appalling death toll from Covid-19.
And in the United States, the United Kingdom and elsewhere, fingers are increasingly being pointed at nursing home workers.
As one recent prominent study puts it, “Nursing home staff are considered to be a source of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in nursing homes.”
Such statements are not only unfair at the individual level; they are also the wrong way to think about how to avoid deaths in the future.
It would be better to face our broader social responsibilities, to consider other sources of viral spread such as hospitals and nursing home visitors, and to spend more resources building trust in public-health systems.
People live in nursing homes either because they are recovering from surgery or because they have a long-term condition that requires continuous medical attention.
Nursing home residents require daily care from trained nurses and other skilled personnel. This is hard work, and when a pandemic arrives, it is dangerous.
Most nursing home staff have gone to great lengths to protect themselves, their families, and the people they care for.
But remember that, at the start of the pandemic, they could not even be provided with properly functioning masks.
Nursing homes were also a low priority for receiving regular Covid-19 tests.
Even as these resource deficits have been addressed and wages have been increased (from initially low levels), many nursing homes remain short of staff.
The people who go to work there every day should be lauded as heroes and provided with every protection imaginable.
Visitors are extremely important to nursing home residents, and the near complete isolation requirements of 2020 were devastating in myriad ways.
However, nursing homes need to be empowered to screen and restrict visitation when it is not safe for vulnerable residents.
With Omicron driving case numbers to new heights, unvaccinated and Covid-positive visitors currently, pose a severe threat to nursing homes.
Hospitals are the crown jewels of any health system, and countries have gone to great lengths – including with costly lockdowns – to keep them functioning.
But hospitals are often held to a different (less demanding) standard than nursing homes, for use of personal protective equipment and testing of employees, patients, and visitors.
The extent of infection control, even in major hospitals, needs the same level of scrutiny as in nursing homes.
Any well-functioning health system needs to ensure the safety of both types of facilities.
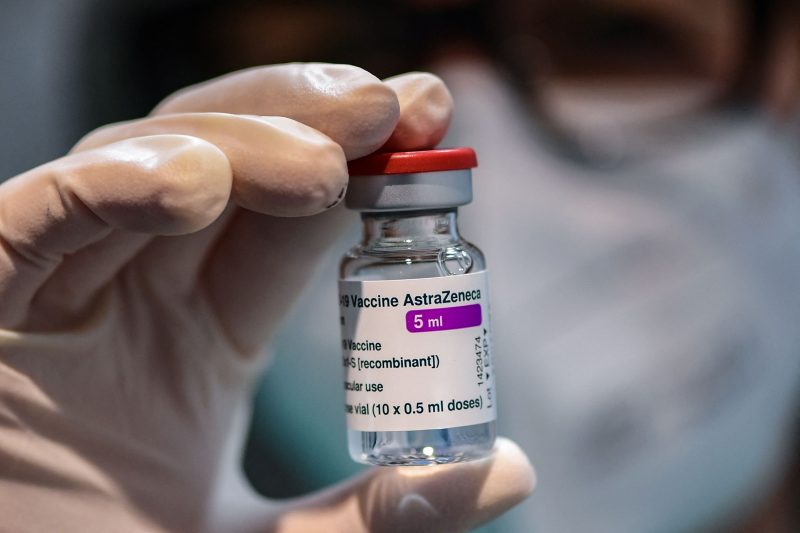
Obviously, we all want the pandemic to go away. The best way to achieve this is to increase the rate of vaccination and to ensure that the uptake of boosters, when appropriate, is as high as possible.
Rates in the US state of Massachusetts are encouraging, including universal vaccination of nursing home staff and the country’s highest rate for boosters.
Massachusetts nursing homes were fortunate to be included in a pilot Covid-19 testing initiative, run by the Broad Institute, as early as April 2020.
This led to a greater understanding of asymptomatic spread and improved infection control across the State.
By August 2020, universal testing protocols for nursing homes were in place, supported financially and logistically by the state’s Department of Public Health.
Currently, all nursing home staff and contractors in Massachusetts must have a weekly PCR test, and when a case is detected, all staff and residents are tested every three days. The state’s nursing homes are also supplied withrapid antigen tests.
Nursing home workers, hospital staff and family members who visit hospitals and nursing homes all contract the virus, primarily from friends and family, with whom they interact indoors, particularly during meals.
Anyone who is not vaccinated is contributing to community spread and increasing the probability that the virus will reach vulnerable people.
Spreading the virus also has a significant economic impact as exposure and infection exacerbates labour shortages.
The greatest current threat to vulnerable residents is lack of staff to care for them.
Misinformation and disinformation have confused people about the value of vaccines, endangering the lives of nursing home workers and vulnerable people everywhere.
Blaming those on the front line of care merely highlights – and compounds – the widespread failure of the public and policymakers to take their responsibilities seriously and behave accordingly. — Article was first published in Project Syndicate















